Substance Misuse and Mental Health - The Challenge of Dual Diagnosis
Functional Links Between Substance Misuse and Mental Health Problems
It can be difficult to convey to clients that their excessive use of alcohol and/or illicit drugs can exacerbate and complicate their mental health problems, increasing the risk of relapse and putting themselves and others at risk. The ideas for this article came from a recent group I facilitated for clients with a diagnosis of schizophrenia. The outline of the group session and some interesting diagrams can be found in my online Prezi presentationSubstance Use and Mental Health.
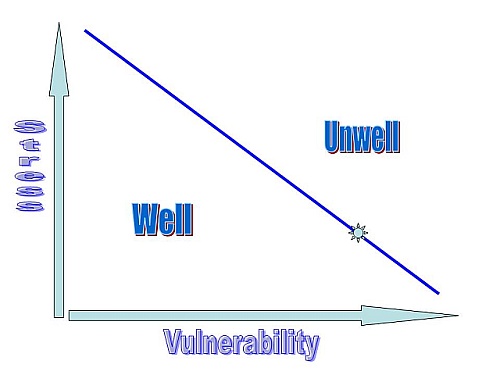
The interactions and links between substance misuse and mental health problems operate in a number of ways, varying from person to person. In some cases it is excessive substance misuse which causes mental health problems in those who are already vulnerable. There are cases of "drug-induced psychosis" (e.g., through the use of amphetamines or cannabis)which resolve once the drug use has stopped. In other cases, the drug use - especially the use of stronger strains of cannabis by younger users(see my Prezi presentation on Cannabis and Mental Health for more details)- acts as a stressor which precipitates a more chronic psychosis in people who have increased vulnerability because of biological/genetic and/or difficult/traumatic environmental factors. This is the stress-vulnerability model in action.
The self-medication hypothesis posits that people use alcohol and drugs as a way to manage their mental health symptoms, either those arising as part of the condition - e.g., to reduce anxiety, OCD symptoms or hearing voices - or to counter the effects of psychotropic medication - e.g.,the use of stimulants such as amphetamines to overcome feelings of lethargy.
It is also possible that the difficulties arise independently - i.e., there is no functional link between the onset of substance misuse and mental health problems. The fourth possibility is that the problems arise from a common factor such as traumatic early life events or current socioeconomis stressors (e.g., homelessness or poverty).
The Biological Substrates of Addiction
It is important to recognise that all substances prone to misuse act on the limbic system which drives our emotions. Here we find the "pleasure centre" or "reward circuit", and its counterpart the periventricular or "punishment circuit". It is the language of pleasure and pain. In simple terms we are motivated to seek pleasure (where we can see drug use as "appetitive" or "positively reinforced") and to avoid pain (where drug use is "negatively reinforced" by taking away both physical and emotional pain). These pathways are powered by a wide range of neurotransmitters, most notably dopamine which is widely recognised as playing an important role in schizophrenia.
Psychological Aspects of Mental Health
We can conceptualise mental health problems as involving disruption in one or more of the following processes:
Furthermore, these are also the processes affected by psychoactive drugs to varying degrees depending on the type of drug and the amount used.
A Simple Analogy for Dual Diagnosis
If I have a broken leg it will create some practical difficulties for me but I should be able to cope with most daily activities by adopting a range of strategies. Similarly, this would also be the case with a broken arm. However, how much more difficult it would be to cope with both at the same time. The strategies I use to cope with the leg might compromise the healing of my arm and vice-versa. This is the challenge of dual diagnosis.
